Streamline Healthcare Fraud Detection for Enhanced Industry Security Using AI
Problem
Manual Healthcare Fraud Detection and its Inefficiencies
Detecting healthcare fraud is a complex and critical task in the healthcare industry. Healthcare providers, insurance companies, and regulatory bodies face the constant challenge of identifying fraudulent claims and activities. The traditional methods of fraud detection are often manual, time-consuming, and prone to errors. These traditional approaches often involve manual review and analysis of extensive sets of data, which can be not only inefficient but also limited in their ability to uncover sophisticated fraudulent activities. ZBrain offers a solution by transforming healthcare fraud detection through advanced artificial intelligence and machine learning.
Solution
I. How ZBrain Enhances Healthcare Fraud Detection
ZBrain automates and improves the healthcare fraud detection process using its advanced AI capabilities. Below is a comparison of the traditional healthcare fraud detection process versus the streamlined process with ZBrain :
|
Steps
|
Without ZBrain Flow
|
Time Without ZBrain Flow
|
With ZBrain Flow
|
|---|---|---|---|
| Data acquisition | Manual | ~6 hours | Automated by ZBrain Flow |
| Data cleaning and preparation | Manual | ~6 hours | Automated by ZBrain Flow |
| Data analysis | Manual | ~8 hours | Automated by ZBrain Flow |
| Report generation | Manual | ~4 hours | Automated by ZBrain Flow |
| Report review and finalization | Manual | ~2 hours | Manual |
| Total | ~26 hours | ~4 hours |
II. Necessary Input Data for Effective Healthcare Fraud Detection
ZBrain Flow relies on specific input data to perform accurate healthcare fraud detection. The following data sources and their associated descriptions are crucial:
| Information Source | Description | Recency |
|---|---|---|
| Electronic Health Records (EHR) | Patient medical history and treatment data, including diagnoses, prescriptions, and medical procedures. | Real-time |
| Claims data | Detailed insurance claims information, billing records, medical services rendered, and financial transactions. | Real-time |
| Provider credentials | Verified medical licenses, certifications, and qualifications of healthcare providers and institutions. | Real-time |
| Pharmacy records | Prescription records and dispensation data. | Real-time |
| Patient demographics | Vital patient information, including demographics, identification, and contact details, is essential for patient identification and communication. | Real-time |
| Fraud databases | Historical repository of healthcare fraud cases and patterns, encompassing data from the past 5 years to identify recurring fraudulent activities. | Last 5 years |
III. How Does ZBrain Work?
Step 1: Data Collection and EDA
ZBrain simplifies the data collection process by automatically acquiring pertinent information for fraud detection. This encompasses a wide range of data, such as medical records, billing information, claims data, and pharmacy records. Once collected, ZBrain undertakes an automated Exploratory Data Analysis (EDA). During this phase, it identifies data patterns and assesses data integrity. ZBrain’s advanced algorithms swiftly process this data, ensuring a comprehensive understanding of the healthcare fraud detection landscape.
Step 2: Embeddings Generation
In this stage, ZBrain transforms textual data, including medical records, billing descriptions, and fraud databases, into numerical embeddings using advanced techniques. These embeddings capture the nuanced relationships within the data, empowering ZBrain to retrieve and analyze information efficiently. These generated embeddings underpin precise analysis, facilitating ZBrain’s ability to identify fraudulent patterns and generate accurate fraud detection recommendations.
Step 3: Query Execution and Action Recommendation
In this stage, when a fraud detection query arises, ZBrain harnesses relevant healthcare data along with user-defined queries and forwards this information to the OpenAI Language Model (LLM). The LLM conducts a comprehensive analysis of the query specifications and the available data to formulate effective fraud detection strategies.
Utilizing advanced embeddings, the LLM tailors fraud detection tactics that consider various aspects, such as patient records, billing history, and claims data. It considers anomalies in billing patterns, unusual treatment procedures, and inconsistencies in patient information. By examining historical data and comparing it to real-time information, the system ensures the detection of irregularities in claims, which helps in preventing healthcare fraud in a precise and timely manner.
Step 4: Parsing and Final Report Generation
Following the formulation of the optimal fraud detection strategies in text format, the next step involves a detailed parsing process. This parsing procedure is designed to extract and organize essential elements, including identified fraudulent patterns, suspect claims, and recommended actions. ZBrain’s detailed parsing technique ensures that the final report is both data-driven and presented in a clear, actionable format, facilitating quick and effective responses from healthcare providers and regulatory bodies.
By automating data collection, analysis, fraud identification and report compilation, ZBrain enhances healthcare fraud detection and empowers organizations to respond swiftly to potential fraud incidents.
Result
Enhancing Healthcare Fraud Detection and Prevention Efficiency
ZBrain transforms healthcare fraud detection by reducing the time and effort required to identify fraudulent activities. The traditional process, which could take up to 26 hours, is streamlined to just around 4 hours with ZBrain, resulting in significant time and cost savings. Using ZBrain, healthcare providers and insurance companies can efficiently detect and prevent fraud, ensuring the integrity of the healthcare system while minimizing financial losses and risks. Embrace the power of ZBrain to fortify the security of your healthcare operations and protect against fraudulent activities.
Example Report
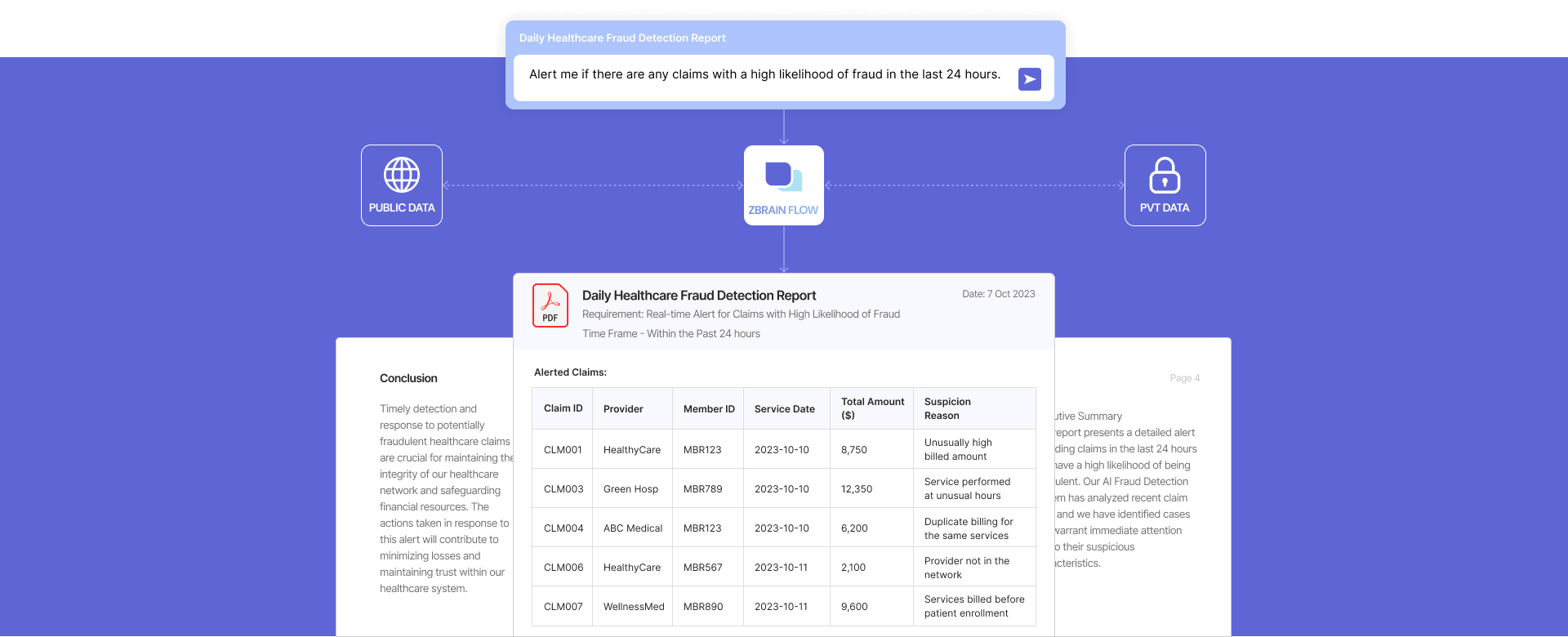
Prompt:
Alert me if there are any claims with a high probability of fraud in the last 24 hours.
Executive Summary
This report presents a detailed alert regarding claims in the last 24 hours that are likely to be fraudulent. Our AI Fraud Detection System has analyzed recent claim data, and we have identified cases that warrant immediate attention due to their suspicious characteristics.
Alert Details
Alert Period:
Last 24 hours (October 27, 2023 – October 28, 2023)
Data Analyzed:
Claims data for the specified time frame, including but not limited to provider information, member information, service dates, total billed amounts, and service descriptions.
Number of Claims Analyzed:
109 claims were processed within the specified time frame.
Claims With a High Likelihood of Fraud:
A total of 7 claims have been identified with a high likelihood of fraud based on the following criteria:
Alerted Claims:
| Claim ID | Provider | Member ID | Service Date | Total Amount ($) | Suspicion Reason |
|---|---|---|---|---|---|
| CLM001 | HealthyCare | MBR123 | 2023-10-27 | 8,750 | Unusually high billed amount |
| CLM003 | Green Hosp | MBR789 | 2023-10-27 | 12,350 | Services performed at unusual hours |
| CLM004 | ABC Medical | MBR123 | 2023-10-27 | 6,200 | Duplicate billing for the same services |
| CLM006 | HealthyCare | MBR567 | 2023-10-28 | 2,100 | Provider not in the network |
| CLM007 | WellnessMed | MBR890 | 2023-10-28 | 9,600 | Services billed before patient enrollment |
Alert Rationale
The AI Fraud Detection System flagged these claims based on various suspicious indicators, including unusually high billed amounts, services performed at unusual hours, duplicate billing, and the engagement of providers not typically seen in our network. It is essential to investigate these claims promptly to prevent potential fraudulent activity and minimize financial losses.
Recommended Actions
- Claims Investigation: Initiate a thorough investigation into each alerted claim to verify the billed services’ accuracy and legitimacy.
- Communication: Contact the providers involved in these claims for additional information and clarification.
- Documentation Review: Review the medical records and supporting documents for each claim to ensure they align with the services billed.
Conclusion
Timely detection and response to potentially fraudulent healthcare claims are crucial for maintaining the integrity of our healthcare network and safeguarding financial resources. The actions taken in response to this alert will contribute to minimizing losses and maintaining trust within our healthcare system.


